Acne
| Audio Version of this Document | Time: 08:14 | Size: 7.7 MB
Publication Date: March 2005
Revised August 2006
What Is Acne?
Publications for the Public
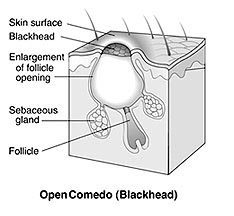
Acne is a disease that affects the skin’s oil glands. The small holes in your skin (pores) connect to oil glands under the skin. These glands make an oily substance called sebum. The pores connect to the glands by a canal called a follicle. Inside the follicles, oil carries dead skin cells to the surface of the skin. A thin hair also grows through the follicle and out to the skin. When the follicle of a skin gland clogs up, a pimple grows.
Most pimples are found on the face, neck, back, chest, and shoulders. Acne is not a serious health threat but, it can cause scars.
- How Does Acne Develop?
- Who Gets Acne?What Causes Acne?
- How Is Acne Treated?
- How Should People With Acne Care for Their Skin?
- What Things Can Make Acne Worse?
- What Are Some Myths About the Causes of Acne?
- What Research Is Being Done on Acne?
How Does Acne Develop?
Sometimes, the hair, sebum, and skin cells clump together into a plug. The bacteria in the plug causes swelling. Then when the plug starts to break down, a pimple grows.
There are many types of pimples. The most common types are:
- Whiteheads. These are pimples that stay under the surface of the skin.
- Blackheads. These pimples rise to the skin’s surface and look black. The black color is not from dirt.
- Papules. These are small pink bumps that can be tender.
- Pustules. These pimples are red at the bottom and have pus on top.
- Nodules. These are large, painful, solid pimples that are deep in the skin.
- Cysts. These deep, painful, pus-filled pimples can cause scars.
Who Gets Acne?
Acne is the most common skin disease. People of all races and ages get acne. But it is most common in teenagers and young adults. An estimated 80 percent of all people between the ages of 11 and 30 have acne outbreaks at some point. Some people in their forties and fifties still get acne.
What Causes Acne?
The cause of acne is unknown. Doctors think certain factors might cause it:
- The hormone increase in teenage years (this can cause the oil glands to plug up more often)
- Hormone changes during pregnancy
- Starting or stopping birth control pills
- Heredity (if your parents had acne, you might get it, too)
- Some types of medicine
- Greasy makeup.
How Is Acne Treated?
Acne is treated by doctors who work with skin problems (dermatologists). Treatment tries to:
- Heal pimples
- Stop new pimples from forming
- Prevent scarring
- Help reduce the embarrassment of having acne.
Early treatment is the best way to prevent scars. Your doctor may suggest over-the-counter (OTC) or prescription drugs. Some acne medicines are put right on the skin. Other medicines are pills that you swallow. The doctor may tell you to use more than one medicine.
How Should People With Acne Care for Their Skin?
Here are some ways to care for skin if you have acne:
- Clean skin gently. Use a mild cleanser in the morning, evening, and after heavy workouts. Scrubbing the skin does not stop acne. It can even make the problem worse.
- Try not to touch your skin. People who squeeze, pinch, or pick their pimples can get scars or dark spots on their skin.
- Shave carefully. If you shave, you can try both electric and safety razors to see which works best. With safety razors, use a sharp blade. Also, it helps to soften your beard with soap and water before putting on shaving cream. Shave lightly and only when you have to.
- Stay out of the sun. Many acne medicines can make people more likely to sunburn. Being in the sun a lot can also make skin wrinkle and raise the risk of skin cancer.
- Choose makeup carefully. All makeup should be oil free. Look for the word “noncomedogenic” on the label. This means that the makeup will not clog up your pores. But some people still get acne even if they use these products.
What Things Can Make Acne Worse?
Some things can make acne worse:
- Changing hormone levels in teenage girls and adult women 2 to 7 days before their period starts
- Pressure from bike helmets, backpacks, or tight collars
- Pollution and high humidity
- Squeezing or picking at pimples
- Hard scrubbing of the skin.
What Are Some Myths About the Causes of Acne?
There are many myths about what causes acne. Dirty skin and stress do not cause acne. Also, chocolate and greasy foods do not cause acne in most people.
What Research Is Being Done on Acne?
Scientists are looking at new ways to treat acne. They are:
- Working on new drugs to treat acne
- Looking at ways to prevent plugs
- Looking at ways to stop the hormone testosterone from causing acne.
For More Information on Acne and Other Related Conditions:
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (226-4267)
TTY: 301–565–2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.gov
The information in this publication was summarized in easy-to-read format from information in a more detailed NIAMS publication. To order the Acne Q&A full-text version, please contact NIAMS using the contact information above. To view the complete text or to order online, visit http://www.niams.nih.gov.
New Treatment of Acne Scarring:
J Eur Acad Dermatol Venereol. 2010 Jun 9. [Epub ahead of print]
Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars.
Aalami Harandi S, Balighi K, Lajevardi V, Akbari E.
Parsian Laser Clinic, Bandar Abbas, Iran.
Abstract
Abstract Background Among therapeutic modalities of acne scars, subcision is a simple, safe procedure with a different  and basic mechanism for correcting atrophic and depressed scars. Subcision releases scar surfaces from underlying attachments and induces connective tissue formation beneath the scar directly, without injury to the skin surface. Therefore, subcision is a valuable method, but due to high recurrence rate, its efficacy is mild to moderate. Objectives To increase the efficacy of subcision, a new complementary treatment of repeated suction sessions was added at the recurrence period of subcised scars. Methods In this before and after trail, 58 patients with mild to severe acne scars of various types (rolling, superficial and deep boxcar, pitted), chicken pox, traumatic and surgical depressed scars were treated by superficial dermal undermining, with mainly 23-guage needles. The protocol for suctioning was: start of suction on third day after subcision for flat and depressing subcised scars and its continuation at least every other day for 2 weeks. Results Forty-six patients followed the protocol completely, had 60-90% improvement in depth and size of scars (significant improvement) with mean: 71.73%. 28.2% of them had ‘80% improvement or more’ (excellent improvement). Twelve patients started suction late and/or had long interval suction-sessions, had 30-60% improvement (moderate improvement) with mean: 43.75%. Conclusion Frequent suctioning at the recurrence period of subcision increases subcision efficacy remarkably and causes significant and persistent improvement in short time, without considerable complication, in depressed scars of the face. Therefore, subcision-suction method is introduced as a new effective treatment.
and basic mechanism for correcting atrophic and depressed scars. Subcision releases scar surfaces from underlying attachments and induces connective tissue formation beneath the scar directly, without injury to the skin surface. Therefore, subcision is a valuable method, but due to high recurrence rate, its efficacy is mild to moderate. Objectives To increase the efficacy of subcision, a new complementary treatment of repeated suction sessions was added at the recurrence period of subcised scars. Methods In this before and after trail, 58 patients with mild to severe acne scars of various types (rolling, superficial and deep boxcar, pitted), chicken pox, traumatic and surgical depressed scars were treated by superficial dermal undermining, with mainly 23-guage needles. The protocol for suctioning was: start of suction on third day after subcision for flat and depressing subcised scars and its continuation at least every other day for 2 weeks. Results Forty-six patients followed the protocol completely, had 60-90% improvement in depth and size of scars (significant improvement) with mean: 71.73%. 28.2% of them had ‘80% improvement or more’ (excellent improvement). Twelve patients started suction late and/or had long interval suction-sessions, had 30-60% improvement (moderate improvement) with mean: 43.75%. Conclusion Frequent suctioning at the recurrence period of subcision increases subcision efficacy remarkably and causes significant and persistent improvement in short time, without considerable complication, in depressed scars of the face. Therefore, subcision-suction method is introduced as a new effective treatment.
PMID: 20553364 [PubMed – as supplied by publisher]
What is Acne?
-
Not to worry, “You will grow out of it”
-
Acne is caused by poor hygiene
-
Acne is caused by something in your diet
-
Vigorous washing helps
-
Treatments don’t work
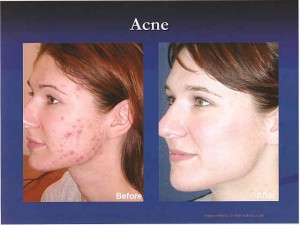
(Photo courtesy of outside source: not actual patient.)
Blu-U Acne Treatments
BLU-U® Blue Light Treatment by Dusa Pharmaceuticals, Inc.
Photodynamic Therapy
Acne Treatment
If you have acne, it can be embarrassing and lead to low self esteem. Without treatment severe cases of acne can be disfiguring, leaving permanent scars. New techniques are available to treat acne and minimize outbreaks.
Acne is an equal opportunity condition, afflicting teenagers, young adults, and occasionally even more mature adults. BLU-U® Blue Light Acne Treatment uses light – without drugs or antibiotics – to treat hard to control acne, including acne vulgaris. The special blue light kills the p. acnes bacterium that grows inside clogged pores that swell up and form pimples on the skin.
BLU-U® light treatments involve sitting with your face close to the light for a short time (typically 8 to 16 mins 40 secs) about once or twice per week for a period of about five weeks or so. The procedure is safe, not painful, and not hot. Over the course of the treatments, most patient experience noticeable control or clearing up of their acne for a very long period.
- Glycolic and or salicylic peels
- Extractions using 30g needle or lancet and comedone extractor
- Slush ( light cryotherpay on swab)
- Microdermabrasion
- Steam, high frequency
1. Wash AM and PM: Wash your face twice daily with:
-
Alternate Benzoyl peroxide wash and Glysal wash. Use one wash in AM (shower) and in the PM (by sink).
-
Ovace face wash, Plexion Cleanser, Rosanil, Clenia.
-
Mild Soap/ Cleanser (Dove, Purpose, Basis, Cetaphil)
- Swipe your face with glysal pad and then rub in a small pea sized amount of Benzoyl peroxide gel on top.
-
Alternative regimens may include:
- Cleocin (clindamycin) lotion, clindet pledget (wipe), clindagel
- Benzac,Brevoxyl, Triaz, Triaz Pad
- Klaron Lotion, Metrogel, Metrolotiom
-
Benzaclin, Duac gel spot treatment
-
Rub in a small pea sized amount of retinol cream over entire face.
-
Alternative regimens may include:
-
Differin gel/cream pledgets to all over face
-
Retin A (tretinoin)
-
Tazorac every night / only every other night to face, back, chest, arms
-
Benzaclin, Duac gel spot treatment, Finacea gel
-
-
One of these antibiotic pills may be prescribed by your dermatologist for 2-6 months:
- Tetracycline
- Minocin/ Minocycline/ Dynacin
- Doxycyline/ Adoxa
-
Amoxicillin
- Zithromax
- Oil-free SPF 30 moisturizer sunscreen for acne prone skin.
-
Alternative Regimens may include:
- Cetaphil or Eucerin lotion for face with sunscreen
- Desowen lotion- once or twice a day ONLY for red itchy rash, dry areas- (don’t use regularly)
-
-
-
Moisturizing sunscreens like Oil-free SPF30 moisturizer sunscreen .
Alternative regimens may include:
-
Gel(non oil) suncreens- Ombrelle, Presun clear gel, solbar liquid, Ti-Screen
-
Best coverage for greater than 15-30 minute sun exposure Obagi Zinc SPF 30, TSC SPF 30 17% zinc
7. If you wear cosmetics make sure they are oil-free and try to avoid powders.
8. If you have any allergic reaction, stop the medication. May use Benadryl pills and hydrocortisone cream over the counter if the rash does not clear. If the rash is severe or the allergic reaction does not clear, call your doctor’s office or go to urgent care.
STOP ALL ACNE PRESCRIPTION MEDICATIONS AND ACNE CREAMS IMMEDIATELY IF DECIDE TO BECOME PREGNANT OR THINK YOU MAY BE PREGNANT.
9. Return for a follow up appointment when suggested by your dermatologist.
10.Recommend The Skin Recovery System (SRS) acne program every 2 weeks including steam, slush, extractions, microdermabrasion and mild glycolic peels. Additional options include blue light, super blue light, or home low level laser treatments.
If unable to see a dermatologist or skin care professional, deeper at home skin cleansing options include an inexpensive home microdermabrasion system called vacubrasion at SkinVacMD.com. Another option includes a sonic, battery operated toothbrush with a soft head (available at Costco) and gently brushing the facial skin in the shower.
-
ACNE & Inflammatory Disorders
- Acne Vulgaris
- Acne Rosacea
- Perioral Dermatitis
- Hidradenitis Suppurativa
- Keratosis Pilaris
- Folliculitis
- Acneiform Dermatitis
Who is Affected?
- Everyone at some time in their life
- From babies to seniors
- high prevalence
- Often under treated or self treated
- Atypical presentations of common disease
- May lead to permanent scarring
- Controllable
Why Treat Acne?
-
Psychosocial impact
-
self esteem, confidence, job, social status
-
Untreated may lead to permanent scarring
-
Emphasis in teenagers -classic occurrence
Dispelling Acne Myths
- Acne is not caused by poor hygiene or diet
- Vigorous washing will not remove comedones and may worsen inflammation
- Topical therapies should be applied to all potential acne areas, not just to lesions, because they work by preventing the formation of new lesions (they do little to shrink existing lesions)
ACNE TRIAD: What makes acne?
-
Follicular plugging (pores closed)
-
Sebum production ( oil production)
-
Bacterial colonization
• Acne is disease caused by 4 interrelated processes affecting the pilosebaceous unit
– altered follicular hyperkeratinization
– sebaceous gland hyperactivity
– Propionibacterium acnes (P acnes) proliferation
– Inflammation/immune hypersensitivity to
P acnes
TRIPLE THERAPY IS KEY!
1. Retinoid (unplugs)
2. Benzoyl peroxide (antibacterial, unplugs,etc)
3. Antibiotics (decrease bacteria)- oral or topical
Combine one product out of each category .
Current Treatment Options
Topical
Retinoids
Benzoyl Peroxide
Antibiotics
Azelaic Acid
Salicylic Acid
Comination treatments
Benzoyl Peroxide + Antibiotics
Oral
Antibiotics
Isotretinoin
Corticosteroids
RETINOIDS
-
Adapal ene
![mpj04394240000[1]](https://lagunaskincenter.com/wp-content/uploads/mpj043942400001-300x201.jpg)