Laguna Hills, CA 92653
Melanoma
At a Glance:
Melanoma is a very common malignancy.
It’s incidence is rising rapidly.
Melanoma is fully curable at early diagnosis
Very poor prognosis for metastatic disease
Close follow-up essential for melanoma patients.
Best prognosis for tumors less than 0.76mm.
MALIGNANT MELANOMA
“Prompt biopsy is key”
May is Melanoma Awareness Month
May is national Melanoma awareness month with several upcoming public awareness and educational programs about this deadly disease. 
We are all familiar with Southern California’s abundance of sun and outdoor activities and its reputation as a hot bed for all types of skin cancers, including
malignant melanoma. The lifetime risk of melanoma is growing higher and is now approximately 1/60-65 individuals. We are seeing more and more
melanomas and very atypical presentations of this malignancy.
The Skin Center will be focusing on Melanoma with our program of comprehensive skin cancer screenings and education starting this month and ongoing though year. If you or your family have concerning lesions, a history of sun burns, fair skin, more than 10-20 atypical moles, or a family history of skin cancer, you or your family member need at least an annual full body skin exam.
This is a very treatable disease when caught in its earliest stages. Most melanomas are found by patients on self- skin exams. Prompt biopsy is key for any suspect new or changing lesions. The American Academy of Dermatology recommends annual full body skin examinations. Adult patients are reminded to have their ANNUAL FULL BODY SKIN CANCER SCAN/ SCREENING. Routine cancer screenings are important for prior skin cancer patients as well as patients with other forms of malignancies. Any new, changing, or suspicious mole should be surgically removed and sent for dermatopathologic exam. When in doubt, it is always best to biopsy a lesion.
May marked national Melanoma awareness month with many educational programs about this disease. We are all familiar with Southern California’s abundance of sun and outdoor activities, and its reputation as a hot bed for all types of skin cancers, including malignant melanoma. The lifetime risk of melanoma is growing higher and is now approximately 1/55 individuals. We are seeing more and more melanomas and very atypical presentations of this malignancy.
We would like to thank you and express our heartfelt appreciation for being a part of our extended family. We understand that you have a choice in healthcare, and we appreciate you choosing us as a part of your trusted family of health care providers. As part of our continued commitment to patient care and service, we are writing you with our annual Melanoma update. We would like to remind you about the importance of proper follow up and care and thank you for your time and dedication to your continued good health.
If you notice any new, changing, growing, itchy moles, or bleeding spots, you should come in right away for a skin check. It is also very important that your family members are continually well educated about atypical moles and melanoma. Currently, full body screenings of close family members by a dermatologist are advised. Remember that early detection of melanoma may be life saving. Most thin melanomas which are detected really early do not spread. The risk of developing a second melanoma is approximately 2-8% in patients with a prior diagnosis of melanoma.
CHECKLIST:
ð Scheduled annual appointment with Dr. Linden or Dr. Jakowatz (714-456-8171) at UCI
ð Scheduled full body skin exam at The Skin Center (949) 582-skin every 6 months
ð Scheduled ophthalmologist for annual eye exam
ð Scheduled annual Gynecologist exam: check for genital moles
ð Scheduled colonoscopy (Age 50 and above) and anal exam
ð Reminded family members to have skin cancer screening at least annually
ð Performed monthly self skin exams, monitoring all moles for any change, or for new moles
ð Use zinc sunscreen SPF 30 daily (Please feel free to stop by The Skin Center to check our selection of specialty zinc based sunscreens)
As always, we look forward to seeing you and would be happy to assist you in any way we can. We wish you the best in your continuing care. If you have any other questions or need to schedule your appointment, please call us at 949-582-SKIN.
 We would like to review some new recommendations from the Scripps Annual Melanoma Conference in San Diego. As always, we’d like to remind you about the importance of proper follow up and care and express our appreciation of your time dedicated to your good health.
We would like to review some new recommendations from the Scripps Annual Melanoma Conference in San Diego. As always, we’d like to remind you about the importance of proper follow up and care and express our appreciation of your time dedicated to your good health.
If you notice any new, changing, growing, itchy moles, or bleeding spots, you should come in right away for a skin examination. It is also very important that your family members are well educated about atypical moles and melanoma. Currently, full body screenings of close family members by a dermatologist are advised. Remember that early detection of melanoma may be life saving.
The risk of melanoma recurrence is higher within 5-8 years after the initial diagnosis. It is important to continue regular follow ups, especially during the first 7-8 years. The major form of melanoma recurrence presents as a lump or bump under the skin, or irregular brown color at the site of the melanoma or close by. Melanoma may metastasize (spread) to lung, liver, brain, etc. Most thin melanomas which are detected really early do not spread. The risk of developing a second melanoma is approximately 2-8% in patients with a prior diagnosis of melanoma. Good routine dermatology check-ups are very important.
1. American Melanoma Foundation (858) 277-4426
2. The National Cancer Institute 1-800-4-cancer
3. American Cancer Society at 1-800-ACS-2345
4. American Academy of Dermatology at www.aad.org.
As always, we will be happy to assist you in any way we can. We wish you the best in your continuing care. We understand that you have a choice in health care and we thank you for choosing us to serve you and your family’s dermatology needs. If you have any other questions or need to schedule an appointment, please call our office 949-582-SKIN.
As you may recall, we traditionally have recommended that every melanoma patient establish baseline care with the UCI Melanoma Center in Orange. Drs. Linden and Jakowatz are excellent and come highly recommended. They have added expertise and are most up to date with respect to the latest advances and improvements in Melanoma. Please call them at (714) 456-8171 or (714) 456-6011. Additionally, Dr. Jakowatz has expertise in a new state-of-the-art mole imaging system called SIA scan, available at UCI.
If you notice any new, changing, growing, or bleeding spots, you should come in right away for a skin examination. It is also very important that your family members are well educated about atypical moles and melanoma. Currently full body screening of close family members by a dermatologist are advised. Remember that early detection of melanoma may be life saving.
Asst. Clinical Professor, Department of Dermatology University of California, Irvine
MELANOMA
Melanoma Overview:
I. Introduction
II. Clinical Aspects
III. Differential Diagnosis
IV. Biopsy techniques
V. Pathology
VI. Current Therapy
VII. Summary
I. Introduction
MELANOMA
Increasingly common malignancy
Incidence rates are rising rapidly
Potentially very lethal
Fully curable at early stage diagnosis
No effective treatments for metastasis
Melanoma
Individual lifetime risk of developing invasive Melanoma:
1935 1 out of 1500 people
1960 1 out of 600 people
1980 1 out of 150 people
2000 1out of 75 people
2010 1out of 50 people
MELANOMA DEFINITION
Malignant transformation of melanocytes
Melanocytes are in the epidermal basal layer
Melanoma can arise de novo or from a pre-existing nevus
Melanoma
Who can get it?
What do I look for?
Can my birthmark become a Melanoma?
How often should I be checked?
II. Clinical Aspects
Skin Cancer is the most common form of cancer in the united states
Melanoma is the most dangerous from of skin cancer. Every hour of every day, someone dies of melanoma in the U.S. and Worldwide
Most frequent sites:
White MALE: back
anterior torso
upper extremity
head and neck
Melanoma
Most frequent sites on females
1. Back
2. Lower leg
3. Arms
4. Head and neck
II. Clinical Aspects
Most frequent sites:
Black and Asian: soles
mucous membrane
palms
nail beds
Melanoma: Soles & Palms
Who is at risk?
RISK FACTORS:
Fair skin, blue eyes, red hair, light complexion
Freckling tendency and inability to tan
Nevi- many or irregular moles, changed moles
Sun exposure and tendency to sunburn
Family History of Melanoma
p16 gene mutation
Prior Melanoma (* several fold increase in risk)
Immunosuppression
Melanoma INCIDENCE:
Represents 3% of all cancers including nonmelanoma skin cancers
Maintained steady increase in incidence over time
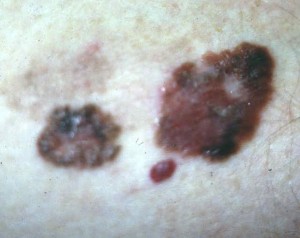
ABCD’s of Melanoma:
MOLES
A= Asymmetry
B=Border irregularity
C=Color variation or change
D=Diameter- bigger than 6mm ( pencil eraser)
E= Evolution- changing lesion
Melanoma is the most common cancer in young adults between ages 20-30 years old
Melanoma is the number 2 cause of cancer death (after breast cancer) in women between ages 30-35 years old.
Presently approximately 1 in 60 people will develop melanoma.
By the year 2010, it is estimated 1 in 50 people will develop Melanoma.
Does Sunlight cause Melanoma?
Causes of most Melanomas are unknown.
Sunlight plays a role in development of some Melanomas, but a direct role in less than half of all melanomas.
Defects and dysregulation in genes play an important role in melanoma, as in all cancers.
Since we don’t understand the pathogenesis of Melanoma, we can only practice sun prevention as our primary prevention at this time.
Melanoma: Rare in Children
Most Melanoma can be cured surgically if detected early.
The prognosis and cure rates are excellent if removed when in situ.
The best way to help prevent skin cancer is protecting yourself from the sun:
Seek shade
Cover up with clothing and hats
Avoid excess sun exposure and sun burning
Apply sunscreen with sun protection factor (SPF) 15 or higher, both UVA and UVB protection.
Biopsy Techniques
MENU of techniques:
Shave biopsy
Tangential shave with 2mm clinical margins
Punch Biopsy
Incisional Biopsy
Excisional Biopsy with 1-5mm margins
Did you know??
Melanoma can rarely occur on
soles
mucous membrane
palms
nail beds
CURRENT THERAPY
SURGERY
SURGERY
SURGERY
The good news….
The cure rate is EXCELLENT if the melanoma is found early.
Five-Year Survival for all melanomas thinner than 0.85mm 99%!
Prevention
1. Education and screening of high risk person
2. Self skin exam
3. Sunscreen use and sun avoidance
4. Specially designed pigmented lesion clinics
5. Mass skin cancer screenings
6. Annual skin exams for melanoma patients
Summary of Melanoma
Melanoma is a very common malignancy.
Its incidence is rising rapidly.
Melanoma is fully curable at early diagnosis
Close follow-up essential for melanoma patients.
Best prognosis for tumors less than 0.76mm.
Sunscreen >SPF15
Sunscreen of at least SPF15 should be used everyday. If you plan to be outdoors for longer periods, then SPF30 is best.
Did you know?
Zinc or Titanium sunscreens are the best sunscreens for physical protection against UVA and UVB.
Follow-up of Melanoma Patients:
All patients with a melanoma should be seen by their dermatologist every three months for the first year. Then they are seen every six months for the next three years. Thereafter, at least once a year full body skin exams are mandatory for best care.
Melanoma- Metastatic Treatment
Limited Treatment Options
Limited Efficacy
Best results are with early surgical intervention
Call to Schedule an appointment at (949) 582-SKIN
For more information, please call (949) 582-7699 or visit the practice website at www.lagunaskincenter.com.
Information in this publication and site is not intended to serve as medical advice. Individuals may use the information as a guide to discuss their treatments with their own physicians. This site does not promote nor endorse the unauthorized practice of medicine by non-physicians or state licensed health care providers.
Medicine is a constantly changing science and not all therapies are clearly established. New research changes drug and treatment therapies daily. The authors, editors, and publisher of these artciles have used their best efforts to provide information that is up-to-date and accurate and is generally accepted within medical standards at the time of publication. However, as medical science is constantly changing and human error is always possible, the authors, editors, and publisher or any other party involved with the publication of this article do not warrant the information in this article is accurate or complete, nor are they responsible for omissions or errors in the article or for the results of using this information. The reader should confirm the information in this article from other sources prior to use. In particular, all drug doses, indications, and contraindications should be confirmed in the package insert.