The Skin Center
Laguna Hills, CA 92653
MOLES
revised 4-18-10
-
What are moles?
· What are risk factors for developing moles?
· Do babies get moles?
· Can I still get new moles as an adult?
· What else could it be?
· What do moles look like?
· What is the difference between a mole and a freckle?
· What types of moles are there?
· What do regular moles look like?
· What do irregular or atypical moles look like?
· Where do irregular or atypical moles commonly occur?
· Are people with freckles more prone to moles?
· What are “liver spots” or “age spots”?
· Are seborrheic keratosis types of moles?
· How can I tell a seborrheic keratosis apart from a mole?
· How do moles develop?
· Who is more prone to getting moles?
· How important is heredity with moles?
· Does having more moles increase my chance of getting melanoma?
· Do moles ever disappear spontaneously?
· Is it dangerous if my mole is getting bigger?
· Should I remove all of my moles?
· Which skin cancers look like moles?
· When should I see a Doctor?
· How often should I check my moles?
· How can moles be prevented?
· When should I start sun protection?
· How can moles be treated?
· Can I remove my moles using Mohs surgery?
· Is there scarring from mole removal?
· Can a plastic surgeon remove my mole?
· Is there pain after mole removal surgery?
· Can my mole grow back after removal?
· Can I go out in the sun after mole removal surgery?
· Is there a blood test or x-ray to diagnose moles?
· What about “UV” cameras that show sun damage?
· Moles At A Glance

What are moles?
Moles are very common small growths that look like a piece of flat or raised skin, and are often tan or brown in color. Most moles are typically the size of a pencil eraser (about 6mm). Moles can range anywhere from pinhead size up to greater than the size of your hand. The medical name for mole is nevus or melanocytic nevus. Multiple moles are called nevi. Essentially, moles are just a collection or clump of pigment cells called melanocytes. While melanocytes normally occur in small numbers in the skin, when these cells bunch up in a nest, they then create what is visible as a mole.
What are risk factors for developing moles?
The most basic risk factor for developing moles is your genetic makeup and the contribution of genes from your parents. Risk factors for getting an increased number of moles also include sun exposure, sunburns, and overall sun damage. The total number of moles on the skin tends to increase with significant sun exposure, and in particular with severe childhood sunburns before the age of 12. The more sun someone gets, the higher the risk of moles in that area. However, moles may also occur in fully sun protected areas like the palms, soles, genitals.
Do babies get moles?
Yes. Moles may be present at birth or gradually appear later in life. Many children continue to develop moles through the teenage years and into young adulthood. Moles tend to grow very slightly in proportion to normal body growth. Congenital moles are moles that are genetically determined. Many of our moles are genetically programmed to appear before we are even born. Other moles may later arise as a result of non-genetic factors like sun exposure.
Can I still get new moles as an adult?
Yes. While many moles arise in the first years of life, the total number of moles typically peaks in the second or third decade of life. Most people do not develop new regular moles after the age of 30. Adults often develop non-mole growths like freckles, lentigines, “liver spots”, and seborrheic keratosis in later adulthood.
New moles appearing after age 30 may require close observation, medical evaluation, and possible biopsy. A brand new mole in an adult may be a sign of an evolving abnormal mole or early melanoma. It is important to have any new or changing mole evaluated by your dermatologist.
What else could it be?
There are many mole look-a-likes including freckles, lentigines, “liver spots”, seborrheic keratosis, melanoma, neurofibroma, hemangiomas, skin tags, and pigmented basal cell cancers. The way to differentiate these other growths is by exam by a dermatologist and possible skin biopsy. Sometimes, a mole may occur adjacent to or on top of a non-mole growth like a freckle or seborrheic keratosis. When in doubt, a skin biopsy can be very helpful in diagnosis.
- · Freckles

- · Lentigines
- · “Liver spots”
- · Seborrheic keratosis
- · Melanoma
- · Neurofibroma
- · Skin tags
- · Hemangioma
- · Pigmented basal cell cancer
- · Café au lait macule
What do moles look like?
Most moles on a person’s skin are usually fairly uniform in color. On different people, moles may vary somewhat in color. Moles may be tan, brown, black, reddish brown, or skin colored. Most moles are about the size of a pencil eraser or the size of your fifth (smallest finger) fingernail. Moles can greatly vary in size from the tiniest pinhead size mole (1mm) to the giant moles that can cover the entire back (10-12 inches). Moles are basically slightly or much darker than the surrounding skin. They also tend to become darker and more apparent with sun exposure and pregnancy, and lighten somewhat in the winter months. Moles can occur anywhere on the body skin including more unusual areas like the scalp, ears, eyelids, lips, palms, soles, genitals, penis, and anal area.
What is the difference between a mole and a freckle?
Both moles and freckles are darker than the surrounding skin. Moles may be raised, slightly raised, or completely flat while freckles are always totally flat. Moles are due to an increase in the total number of pigment cells called melanocytes. Freckles and “liver spots” are due to an increase in the amount of dark pigment called melanin. Although both tend to occur more frequently on sun damaged skin, moles can occur in totally sun protected areas.
What types of moles are there?
There are 3 basic types or groups of moles: regular, irregular, and cancerous. Irregular moles are also called atypical moles, dysplastic nevi, or Clark’s nevi. Regular moles are typically benign and friendly. Irregular moles have some irregular or abnormal cells that have a potential to change or become cancerous over time. Irregular moles do not always turn into melanoma or cancer. Cancerous moles like melanomas are highly irregular and have already become malignant. A small number of regular moles may potentially evolve and become irregular or cancerous over time. It is important to watch all moles closely for change or atypical features. Monthly self skin exams and at least annual full body moles exams by a dermatologist are important in the early detection of abnormal moles and melanoma.
- · Regular moles
- · Irregular (or dysplastic) moles
- · Cancerous moles
What do regular moles look like?
Regular moles are usually symmetrical, have regular borders, uniform color, and are about the size of a pencil eraser or smaller. Regular moles may be flat or raised. While regular (noncancerous) moles more commonly may have associated hairs, essentially any mole may have hair. The presence or absence of hair does not necessarily differentiate regular versus irregular moles.
- · Symmetrical
- · Regular borders
- · Uniform color
- · Smaller than a pencil eraser
- · Unchanged and present for a long time
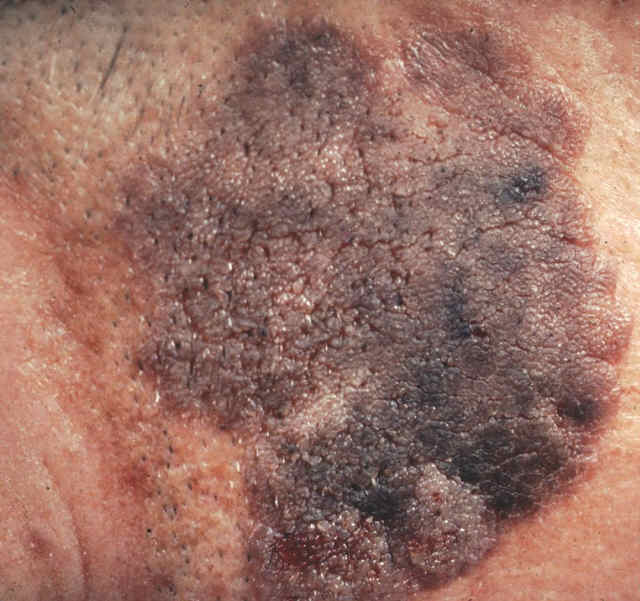
What do irregular or atypical moles look like?
Irregular or atypical moles are usually asymmetrical, have irregular borders, multiple or dark colors, and bigger that the size of a pencil eraser. Irregular moles are most often flat or nearly flat. This is one of the most important distinctions between regular and irregular moles and most often misunderstood by most people. While most people go to their doctors or dermatologist for raised moles, it is actually the flat moles that are the most medically concerning. Having more than 20-25 irregular or dysplastic moles may increase the person’s overall risk of developing melanoma. The presence of a giant congenital mole greater than approximately 8-10 inches in size also may infer an increased risk of melanoma.
- · A-Asymmetrical
- · B- Irregular borders
- · C-Multiple colors
- · D- Diameter bigger than a pencil eraser
- · E- Evolving ,changing, or new
Where do irregular or atypical moles commonly occur?
Irregular moles can occur anywhere on the body but are most common on sun exposed skin, especially on the upper back and shoulders where people frequently get their most severe sunburns. The risk of melanoma is greater on sun damaged skin like the shoulders, upper back, and head and neck. Ears are particularly a common site of atypical moles because of the difficulty in applying sunscreen and frequent sun exposure. Women have increased risks of atypical moles particularly on the lower leg and calf. Any new or changing irregular mole on a woman’s calf warrants immediate medical evaluation.
Are people with freckles more prone to moles?
Yes. Moles are more common in people prone to freckles. Freckles, also called ephelides, are flat spots that are tan, slightly reddish or light-brown and typically appear during the sunny months. They are most often found in people with light complexions and in some families, they are a hereditary (genetic) trait. Many people with reddish hair and green or blue eyes are more prone to these types of skin growths. Sun avoidance and sun protection, including the regular use of sunscreen may help to suppress the appearance of the some types of moles and freckles.
What are “liver spots” or “age spots”?
“Liver spots” or “age spots” are the common names of the darker spots seen in adults, frequently on the back of the hands. Liver spots are not true moles or freckles. The term “liver spot” is actually a misnomer since these spots are not caused by liver problems or liver disease. While these do tend to appear over time, they are not in themselves a sign of old age. Instead, they appear generally on sun-exposed areas, more so in people who have a genetic tendency to develop them. They are commonly seen on the skin of older adults with a history of sun exposure. Liver spots are simply the result of a localized increase in the number of melanosomes (normal pigment carrying particles in cells).
Are seborrheic keratosis types of moles?
No, seborrheic keratosis (SK) are not true moles. Moles are caused by an increased number of melanocytes. Seborrheic keratosis are caused by a small area of thickening of the epidermis and do not involve melanocytes (pigment cells).
Seborrheic keratoses are also benign (not malignant) growths of the skin. Some people call these growths “barnacles” or “Rice Krispies”. Although they are most often medium brown, they can differ in color ranging anywhere from light tan to black. They occur in different sizes, too, ranging anywhere from a fraction of an inch (or centimeter) to an inch (2.5 cm) in diameter. Typically these growths are around the size of a pencil eraser or slightly larger. Some keratoses begin as a flat lentigo and gradually raise and thicken to form a seborrheic keratosis. A biopsy may in some cases be required to distinguish a seborrheic keratosis from an irregular mole or melanoma.
How can I tell a seborrheic keratosis apart from a mole?
The telltale feature of a seborrheic keratosis is its waxy, stuck-on, greasy look. Seborrheic keratosis can almost be peeled or scraped off the skin while moles are not easily scraped. Seborrheic keratoses look like they have either been pasted on the skin or may look like a dab of melted brown candle wax that dropped on the skin. Seborrheic keratosis may occur in the same areas as moles. Seborrheic keratoses are also more common in areas of sun exposure, but may rarely occur in doubly sunprotected areas like the underwear area. When they first appear, the growths usually begin one at a time as small rough bumps. Eventually, they may thicken and develop a rough, warty surface.
Seborrheic keratoses are quite common especially after age 40. Almost everybody may eventually develop at least a few seborrheic keratoses during their lifetime. These growths are sometimes referred to as the “barnacles of old age.”
How do moles develop?
Moles are thought to develop primarily from genetics, and secondly from a combination of genetic tendency and sun exposure in some individuals. Moles form from a nest or group of melanocytes in the epidermis. Two people receiving the same sun exposure may not have an equal chance of developing moles. Natural sunlight and artificial sun-tanning lights emit ultraviolet (UV) rays. After exposure to ultraviolet rays, the outer layer of the skin (the epidermis) thickens and the pigment-producing cells (the melanocytes) produce the pigment melanin at an increased rate. (This production of melanin may in fact give some protection against future sun exposure.)
Who is more prone to getting moles?
People differ a great deal in their propensity to developing moles and reaction to sunlight. To take an extreme example, there is no pigmentation in the skin of an albino because of a defect in melanin metabolism. On the other hand, people with dark complexions are relatively less sensitive to sun exposure than fair-skinned persons. However, persons with dark skin are not entirely resistant to the effects of the sun, and they, too, can become sunburned with prolonged exposure. Persons with blonde or red hair, light colored eyes, and fair skin are especially susceptible to the damaging effect of UV rays.
- · Fair skin
- · Light eyes
- · Red hair
- · Freckled
- · Sun sensitive
- · Easy sunburn
Irrespective of skin color, moles are caused by a local clumping or nest of mole cells in the epidermis. A Mole is essentially nothing more than a group of nested melanocytes at one spot in the skin.
How important is heredity with moles?
Heredity (your genetics) and skin type are very important in the tendency to develop moles. Some moles tend to be inherited genetically in everyone and are predetermined before birth. Moles are seen in all races and skin colors from Caucasian, Asian, African, and Indian. Moles are also seen in animals like dogs. Individuals with fair skin and blond or red hair are more prone to developing moles.
Twin studies, including pairs of identical twins and pairs of fraternal (non-identical) twins, have found a striking similarity in the total number of moles found on each pair of identical twins. Such similarities were considerably less common in fraternal twins. These studies strongly suggest that the occurrence of moles is influenced by genetic factors. In fact, the variations in mole counts appear to be due largely to heredity.
Ongoing research in a rare disease called Xeroderma Pigmentosum has also confirmed the genetic tendency of moles. Excessive moles in dark haired individuals are quite common in this disease. Further, increased pigment is also found in skin folds like the underarms in another uncommon genetic disease called Neurofibromatosis.
Does having more moles increase my chance of getting melanoma?
Yes. The total number of irregular moles on your body is one of the strongest indicators for the risk of developing a malignant melanoma. There is also a direct relationship between the number of innocent moles on the skin and the chance of developing an abnormal or changing mole. The more moles you have, the greater the risk of developing atypical moles and potentially melanoma.
Do moles ever disappear spontaneously?
Yes. In rare cases, some moles may lighten or completely disappear later in life. In some cases, this is the result of the body’s immune system stacking the mole and causing it to regress. One example of this is a “halo nevus”. A biopsy may be required to exclude atypical cells in these types of moles.
Is it dangerous if my mole is getting bigger?
New or enlarging moles may be concerning and should be promptly evaluated by your dermatologist. While moles may increase in size, particularly before the age of 20, regular moles are unlikely to enlarge as people get older. A mole that has increased in size is not necessarily cancerous. Enlargement alone does not necessarily mean a mole is malignant. Some regular moles may increase in size and darken in pregnancy. Often, a simple mole biopsy by your doctor can help determine if a mole is irregular.
Should I remove all of my moles?
No. Regular moles pose essentially little to no health risk. It is not necessary to remove all of your moles. Most moles are not cancerous and generally do not become cancerous. However, moles that are changing, growing, new, symptomatic, bleeding or otherwise worrisome to your physician or dermatologist may need to be removed and tested for irregular cells. Periodic monitoring and medical evaluation of moles is important to help determine which moles need to be removed. If you have a family history of melanoma, greater attention should be paid to your moles and an overall lower threshold for biopsy of irregular moles.
Which skin cancers look like moles?
Melanoma — This very dangerous form of skin cancer may appear even in young people and on parts of the body that are sun exposed as well as those that are protected. While the exact cause of melanoma is not entirely known, genetics and ultraviolet rays (particularly UV-A) are known to play a part. Melanomas may arise from a previously normal mole or pigmented spot that has been present many years or lifelong. Melanomas may also arise from completely normal skin without an apparent pre-existing mole. In comparison with benign (non-cancerous) moles, melanomas tend to be larger, darker, and have more irregular color and shape variations. Most melanomas are actually flat and not raised as many people tend to incorrectly assume.
Lentigo maligna (“malignant Mole”) — This is an uncommon fairly superficial skin cancer that generally occurs on the faces of older adults who have a history of considerable sun exposure. Over the course of months to years, this condition may, if untreated, develop into a more aggressive malignant variety called lentigo maligna melanoma. There are of course many hundreds of ordinary facial moles for every one that is potentially malignant. A simple in-office test called a skin biopsy can help diagnose lentigo maligna.
Basal cell carcinoma — This is the most common type of skin cancer. These are usually pearly, pink or reddish in color and may bleed easily. Pigmented basal cell carcinoma is a type of basal cell that may be confused for a mole or seborrheic keratosis because of its brown or dark color. A simple procedure called a skin biopsy can help diagnose this growth.
When should I see a Doctor?
Anyone who has one or more uncertain moles or pigmented spots should have their physician or dermatologist evaluate them. Even verbal descriptions and photographs cannot convey enough information for satisfactory self-diagnosis. As always, it is better to be safe than sorry. Routine annual mole checks are an important part of your general health screenings. Birthdays are a good time to remember to schedule your annual “birthday suit” mole check. Since existing moles may change and new growth arise, periodic rechecks are necessary.
How often should I check my moles?
The American Academy of Dermatology recommends monthly self skin exams and a full body skin examination for adults as part of a routine annual health exam. It is important to have any new, changing, bleeding mole or growth examined by your physician or dermatologist as soon as possible. Skin cancers, including melanomas, are generally curable if diagnosed and treated at an early stage.
How can moles be prevented?
Since we can not change our own genetics, it is not possible to prevent all moles. Our main prevention measures are aimed at sun avoidance and sun-protection including:
1. Use of sunscreens with SPF (sun protection factor) 30
2. Use of wide brimmed hats ( 6 inches)
3. Use of sun protective clothing ( shirts, long sleeves, long pants)
4. Avoidance of the peak sun hours of 10am to 4pm
5. Seeking shade and staying indoors.
Ideally mole prevention is more effective that later trying to remove moles that have already developed. Mole removal will leave some type of scar at the site of the prior mole. Smaller moles are easier to remove and leave less scars. Larger mole removal may be more difficult and not always satisfactory in cosmetic scar appearance.
When should I start sun protection?
Everyone, especially those with known hereditary tendencies of freckling, should start sun protection early in childhood. Much of the sun and UV skin damage occurs often while children are under age 18.
Fair skin people who are more prone to freckling an sunburns are also generally more at risk for developing moles and skin cancers. Sun sensitivity and easy burning may be a warning sign of sensitive skin which is highly vulnerable to sunburn and to potential skin cancer.
How can moles be treated?
True moles can be treated by surgical removal. Moles cannot be treated by fading or lightening creams, bleaches, freezing, or other chemicals. Moles can easily be removed by fairly minor, in-office procedures including shave removal, punch biopsy, or full surgical excision.
Regular moles do not necessarily have to be treated. Changing or medically concerning moles need to be fully, surgically removed and sent to a lab for special tissue examination called pathology.
Some people like their moles while others may be more bothered by their appearance. The cosmetic improvement of the skin is a frequent request among people with moles. Moles are desirable by some people who like the special character or uniqueness these give them like Cindy Crawford. Other moles may have potential negative social perceptions or stigma.
Although lasers may be used in some countries and by some medical centers to remove some types of moles, laser treatments are not recommended for irregular moles. Irregular moles need to be surgically removed and the tissue sent for testing to make sure all the atypical cells are cleared. Lasering the surface of an irregular mole may inadvertently delay or make potential detection of melanoma much more difficult. While sun spots or lentigines may respond to bleaching or fading creams, freezing with liquid nitrogen, laser, intense pulse light, and chemical peels, true moles are not removable by these methods.
Can I remove my moles using Mohs surgery?
No, Mohs surgery is not for mole removal. It is primarily designed for removing skin cancers. Moles are usually removed by standard or traditional surgery. The rapid freezing technique used for Mohs surgery tends to distort mole cells and may make the removed tissue more difficult to examine under the microscope.
Is there scarring from mole removal?
Yes, all human beings heal by permanent scar formation. In general, when you cut the skin, there will be some type of scar. Some people heal better than others. Some scars are more noticeable depending on the location and skin type.
There are many options for treatment of surgical scars including lasers, scar creams and gels, cortisone injections, and many other choices depending on the scar. You may want to discuss ways to help minimize scarring with your doctor at your stitch removal appointment.
Can a plastic surgeon remove my mole?
Yes. You may decide to have your mole removal with a plastic surgeon especially if the mole is on your face or other cosmetic area. Plastic surgeons may have additional and specialized training in cosmetic skin growth removal. Regardless of what type of doctor removes your mole, it is important to keep in mind that all mole removals will leave some type of scar.
Is there pain after mole removal surgery?
Most people report no or minimal discomfort after mole removal surgery and require no pain medication. If there is pain, many people find that they prefer to take something for pain at the first hint of discomfort instead of waiting until the pain builds up to an unbearable level. If you have mild or moderate pain, your doctor may advise you to take Tylenol (Acetaminophen) or another pain reliever over the counter. Aspirin or Aspirin containing pain relievers may cause increased bleeding. Rarely, prescription pain medications may be required for severe pain.
Can my mole grow back after removal?
Yes. Depending on how it was removed, there is a small chance that your mole can recur after mole surgery. Lasered moles often recur.
It is important to understand that no surgery has a 100% removal rate. A few mole cells may remain in the skin and may recur in the same or adjacent area. Some moles are more aggressive than others and need additional treatment and closer follow up.
Good follow up appointments with your physician are very important, especially in the first few years after irregular mole removal. Many people are seen every 6-12 months after their diagnosis of atypical moles. More regular follow up appointments may be needed for those with more aggressive moles or moles in high risk areas. Your physician will recommend the proper follow up for your specific condition.
Can I go out in the sun after mole removal surgery?
Yes. There are no specific strict sun restrictions after mole removal surgery. You may go out in the sun with sunscreen and protective hats and clothing. Overall, the sun is not your friend and should be avoided in excess. Excess sun exposure has been linked to possible melanoma. Use of sunscreen or other cover up on the scar is very helpful for at least 6 months after surgery to help minimize scarring. It is important to follow your own physician’s instructions for wound care and sun protection.
Is there a blood test or x-ray to diagnose moles?
No. There are no blood tests or special x-rays for moles.
There are however newer digital mole images like the SIA scan (SIA = Spectrophotometric Intracutaneous Analysis) or SIAscopy that are now available to help image moles. These non-invasive, computerized mole scan devices can help objectively examine a mole and capture information like size, amount and pattern of pigment, blood flow, and other characteristics. Based on this information, changes in moles or irregular cells may be more readily identified. This technology is fairly new and still developing.
What about “UV” cameras that show moles?
UV cameras using special black and white images depicting the amount of sun damage may be helpful in some cases to demonstrate sun damage. UV cameras do not diagnose moles or skin cancer.
Moles At A Glance
- Moles are common, small tan or brown spots on the skin.
- Moles may be flat or raised.
- Most moles are genetically pre-determined before we are born.
- Sun exposure in childhood causes an increase in number of moles.
- Most moles appear by age 20 or 30.
- Moles may be mistaken for freckles and other skin growths.
- Irregular moles may develop into skin cancer called melanoma.
- Skin cancer may at times masquerade or hide as a regular mole.
- Irregular or changing moles should be promptly examined by your physician or dermatologist.
- Minor surgery is the most effective way to remove a mole.
For more information, please call (949) 582-7699 or visit the practice website at www.lagunaskincenter.com.
Information in this publication and site is not intended to serve as medical advice. Individuals may use the information as a guide to discuss their treatments with their own physicians. This site does not promote nor endorse the unauthorized practice of medicine by non-physicians or state licensed health care providers.
Medicine is a constantly changing science and not all therapies are clearly established. New research changes drug and treatment therapies daily. The authors, editors, and publisher of these artciles have used their best efforts to provide information that is up-to-date and accurate and is generally accepted within medical standards at the time of publication. However, as medical science is constantly changing and human error is always possible, the authors, editors, and publisher or any other party involved with the publication of this article do not warrant the information in this article is accurate or complete, nor are they responsible for omissions or errors in the article or for the results of using this information. The reader should confirm the information in this article from other sources prior to use. In particular, all drug doses, indications, and contraindications should be confirmed in the package insert.

